CT Head Interpretation
- CT Head Basic Interpretation in Spanish [Lawrence B. Stack, MD]
The CT head scan is a computer-generated series of images from multiple X-rays taken at different levels. Fine X-ray beams passed through the subject are absorbed to different degrees by different tissues and the transmitted radiation is measured by a scanning device.
The degree of absorption of X-rays is proportional to the density of the tissue through which it passes. Hounsfield units (HU) are used to measure how much of the X-ray beam is absorbed by the tissues at each point in the body. The denser the tissue, the more the X-ray beam is attenuated and the higher the number. Units are established on a relative scale with water as the reference point. Water is always 0 HU, bone is approximately 1000 HU and air is –1000 HU
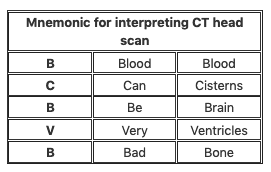
Interpretation
Use a systematic approach to viewing the anatomical structures in the many slices prepared by the CT scanner.
- Orientation
- The CT slice is regarded as being viewed from the patient’s feet, so the left side of the picture as you view it is the right side of the patient.
- Contrast versus non-contrast
- Determine if scans have been taken with or without IV contrast, as contrast may mimic the presence of blood. IV contrast does not cross the normal blood brain barrier and is used if there is a suspicion of tumour, infection (e.g. abscess) or vascular abnormality (e.g. AVM or aneurysm)
- General review
- Generate a system to review all the essential features of the CT head scan
Blood
- Look for the presence of blood. Clues to the origin of the haemorrhage, its duration and the cause of the insult may be indicated by its position and spread.
- Acute haemorrhage absorbs X-rays and appears hyperdense (white) on CT scans. As the clot retracts it becomes more hyperdense over the first few hours up to 7 days; then isodense with brain over the following 1-4 weeks and finally hypodense compared with brain over the subsequent 4-6 weeks.
- Extracerebral (axial) haemorrhage occurring within the skull, but outside the brain
- Extradural haemorrhage (EDH) – biconvex lesion that does not cross suture lines; usually secondary to arterial injury.
- Subdural haemorrhage (SDH) – crescent-shaped blood collection that can cross suture lines; usually secondary to venous disruption of surface and/or bridging vessels.
- Subarachnoid haemorrhage (SAH) – haemorrhage into the CSF and cisterns secondary to aneurysms, trauma and arteriovenous malformation.
- Intracerebral (axial) haemorrhage occurring within the brain itself
- Intracerebral haemorrhage (ICH) – secondary to trauma, hypertension and haemorrhagic stroke.
- Intraventricular haemorrhage (IVH) – usually associated with significant trauma.
Cisterns
- Cisterns are collections of CSF, which surround and protect the brain. Examine each for evidence of effacement, asymmetry and the presence of blood.
- Circum-mesencephalic—surrounding the midbrain
- Suprasellar—around the circle of Willis
- Quadrigeminal—located at the top of the midbrain
- Sylvian—between temporal and frontal lobes.
Brain matter
- Compare the sulcal pattern (gyri) for evidence of effacement and relative volumes of the left and the right sides of the brain for asymmetry. Trace the falx through the series of scans, looking for mid-line shift secondary to compartmental mass effect.
- Look for inconsistencies in the grey–white differentiation (e.g. evolving embolic stroke). Patients with CVA may have a normal CT head scan on presentation with subtle oedema beginning at 6-12 hours, hypoattenuation after 24 hours and maximal oedema at 3-5 days.
- Identify hyperdense regions associated with blood, IV contrast or calcification.
- Identify hypodense regions associated with air, fat, ischaemia or tumour.
Ventricles
- Examine the lateral ventricles, 3rd and 4th ventricles for asymmetry, dilatation (hydrocephalus), effacement and haemorrhage.
Bone
- Cortical bone has the highest density on the CT scan (300–1000 HU) and is best viewed on separate bony windows when looking for evidence of fractures or tumours.
References and Links
CCC Neurocritical Care Series
Emergencies: Brain Herniation, Eclampsia, Elevated ICP, Status Epilepticus, Status Epilepticus in Paeds
DDx: Acute Non-Traumatic Weakness, Bulbar Dysfunction, Coma, Coma-like Syndromes, Delayed Awakening, Hearing Loss in ICU, ICU acquired Weakness, Post-Op Confusion, Pseudocoma, Pupillary Abnormalities
Neurology: Anti-NMDA Encephalitis, Basilar Artery Occlusion, Central Diabetes Insipidus, Cerebral Oedema, Cerebral Venous Sinus Thrombosis, Cervical (Carotid / Vertebral) Artery Dissections, Delirium, GBS vs CIP, GBS vs MG vs MND, Guillain-Barre Syndrome, Horner’s Syndrome, Hypoxic Brain Injury, Intracerebral Haemorrhage (ICH), Myasthenia Gravis, Non-convulsive Status Epilepticus, Post-Hypoxic Myoclonus, PRES, Stroke Thrombolysis, Transverse Myelitis, Watershed Infarcts, Wernicke’s Encephalopathy
Neurosurgery: Cerebral Salt Wasting, Decompressive Craniectomy, Decompressive Craniectomy for Malignant MCA Syndrome, Intracerebral Haemorrhage (ICH)
— SCI: Anatomy and Syndromes, Acute Traumatic Spinal Cord Injury, C-Spine Assessment, C-Spine Fractures, Spinal Cord Infarction, Syndomes,
— SAH: Acute management, Coiling vs Clipping, Complications, Grading Systems, Literature Summaries, ICU Management, Monitoring, Overview, Prognostication, Vasospasm
— TBI: Assessment, Base of skull fracture, Brain Impact Apnoea, Cerebral Perfusion Pressure (CPP), DI in TBI, Elevated ICP, Limitations of CT, Lund Concept, Management, Moderate Head Injury, Monitoring, Overview, Paediatric TBI, Polyuria incl. CSW, Prognosis, Seizures, Temperature
ID in NeuroCrit. Care: Aseptic Meningitis, Bacterial Meningitis, Botulism, Cryptococcosis, Encephalitis, HSV Encephalitis, Meningococcaemia, Spinal Epidural Abscess
Equipment/Investigations: BIS Monitoring, Codman ICP Monitor, Continuous EEG, CSF Analysis, CT Head, CT Head Interpretation, EEG, Extradural ICP Monitors, External Ventricular Drain (EVD), Evoked Potentials, Jugular Bulb Oxygen Saturation, MRI Head, MRI and the Critically Ill, Train of Four (TOF), Transcranial Doppler
Pharmacology: Desmopressin, Hypertonic Saline, Levetiracetam (Keppra), Mannitol, Midazolam, Sedation in ICU, Thiopentone
MISC: Brainstem Rules of 4, Cognitive Impairment in Critically Ill, Eye Movements in Coma, Examination of the Unconscious Patient, Glasgow Coma Scale (GCS), Hiccoughs, Myopathy vs Neuropathy, Neurology Literature Summaries, NSx Literature Summaries, Occulocephalic and occulovestibular reflexes, Prognosis after Cardiac Arrest, SIADH vs Cerebral Salt Wasting, Sleep in ICU
Critical Care
Compendium
