Examination of the unconscious patient
Reviewed and revised 30 March 2015
OVERVIEW
Coma
- Coma is a state of unconsciousness caused by temporary or permanent impairment of the ascending reticular system in the brainstem, or both cerebral hemispheres.
The key components of the neurological examination of the comatose patient are:
- level of consciousness (Glasgow Coma Score — list the components; e.g. E4V5M6 = GCS 15)
- the pattern of breathing
- size and reactivity of the pupils
- eye movements and oculovestibular responses
- motor responses (tone, reflexes and posturing)
- meningism and signs of the underlying cause
In particular, assessment of asymmetry for the presence of focal neurological deficits is vital.
CAUSES OF COMA
Causes with focal signs
- no meningism — stroke, space occupying lesions (e.g. tumor, hemorrhage, abscess), injury, inflammation
- meningism — meningoencephalitis, subarachnoid haemorrhage (SAH)
Systemic causes without focal signs (TOMES)
- Toxins
- Organ failures
- Metabolic — check COATPEGS (CO2, O2, ammonia, temperature, pH, electrolytes, glucose, serum osmolality)
- Endocrine
- Seizures
Remember that systemic causes can sometimes have focal signs! (e.g. Todd’s paresis, hemiparesis due to hypoglycemia)
GENERAL EXAMINATION
General examination is also important
- consider the neurological findings in light of the vital signs, evidence of trauma, acute or chronic illness, and/or drug ingestion
- cranial scars, drains, ICP monitors and VP shunts
- neck stiffness
- track marks and drug paraphernalia
- infusions (e.g. sedatives, nimodipine, vasopressors)
- ventilator (evidence of spontaneous breaths?)
LEVEL OF CONSCIOUSNESS
- GCS is most commonly used (see Glasgow Coma Scale (GCS))
- Other scores such as the Richmond Agitation-Sedation Score (RASS) are used to titrate sedation (see Sedation in the ICU)
PATTERN OF BREATHING
Breathing pattern is often forgotten in intubated patients, but is important as the pattern of breathing correlates with the level of the lesion, and may suggest other causes
- Cheyne-Stokes Respiration is not specific but is seen in lesions above the brainstem
- Central hyperventilation, or prolonged inspiratory pauses or irregular ataxic breathing indicates various brainstem lesions as does apnea
- Also look for deep rapid Kussmaul breathing, secondary to a metabolic acidosis, as in diabetes ketoacidosis
- Look for spontaneous breaths in the ventilated patient (may be suppressed if hyperventilated)
PUPILLARY RESPONSES
- We need to assess the pupils for size, asymmetry and reactivity to light
- Different sized pupils correspond to different types of lesions
- pinpoint pupils occur in pontine lesions and certain overdoses (e.g. opioid, clonidine)
- fixed mid-sized pupils occur in midbrain lesions
- One dilated pupil suggests CN3 compression – e.g. ICH, PCOM aneurysm or raised ICP (parasympathetic nerves are in the superficial parts of the nerve, so tend to be more vulnerable to compressive lesions – ptosis and ‘down and out’ eye positioning tends not to occur due to sparing of the more central motor fibers)
OCULAR DEVIATION AND DYSCONJUGATE GAZE
Dysconjugate gaze
- Most individuals have a degree of exophoria when drowsy for any reason and any underlying strabismus tends to worsen
- thus dysconjugate gaze is difficult to interpret in the stuporous or comatose patient
Tonic deviation
- A frontal lobe lesion on the same side as the eye deviation, commonly a stroke. This can also be a result of a Todd’s paralysis following a seizure (whereas during the seizure the eyes deviate in the opposite direction — away from the origin of the ‘irritative’ focus).
- A pontine lesion on the opposite side to the eye deviation. ‘Wrong way eyes’ may also be seen in thalamic hemorrhage.
- Lateral gaze deviation from a pontine lesion cannot be overcome by stimulating oculocephalic or oculovestibular reflexes (see below), whereas supranuclear (e.g. frontal lesions) can. Hence they can be distinguished clinically.
Skew deviation
- Vertical separation of the ocular axes is called skew deviation
- This is suggestive of a pontine or vestibulocerebellar lesion on the side of the inferior eye, or a medial longitudinal fasciculus lesion on the side of the superior eye
Abnormal eye position can also result from cranial nerve palsies (CN6 is particularly at risk due to it’s long course) and orbital entrapment in trauma
OCULOVESTIBULAR REFLEXES
Oculocephalic reflex (‘doll’s eye’ reflex)
- ensure the C-spine is cleared
- the patient’s eyes are held open
- the head is briskly turned from side to side with the head held briefly at the end of each turn
- a positive response occurs when the eyes rotate to the opposite side to the direction of head rotation, thus indicating that the brainstem (CN3,6,8) is intact
- a similar result is seen when the head is flexed and extended — a positive result is downward deviation of the eyes during extension, and upward deviation during flexion (the eyelids, if closed, may also open as part of the ‘doll’s head phenomenon’). These vertical responses indicates that the brainstem (CN3,4,8) is intact
- The eyes should gradually return to the mid-position in a smooth, conjugate movement if the brainstem is intact
- Patients with metabolic coma (e.g. hepatic failure) may have exaggerated, brisk oculocephalic reflexes
Oculovestibular reflex (caloric stimulation)
- the head is elevated to 30 degrees above horizontal so that the lateral semicircular canal is vertical, and so that stimulation with generate a maximal response
- check that the tympanum is intact and that the external ear canal is clear — C-spine clearance is not necessary
- introduce iced water into the external ear canal through a small catheter until one of the following occurs:
— nystagmus (in the intact brainstem the slow phase is towards the irrigated ear)
— ocular deviation
— 200mL of iced water has been instilled - allow 5 minutes between testing ears to allow re-equilibration of the oculovestibular system
- as consciousness is lost, the fast component (towards the non-irrigated ear) is lost and the slow component tonically deviates the eye in the direction of the irrigated ear
Vertical oculovestibular eye responses can be assessed by irrigated both ears simultaneously
- If the brainstem is intact, cold water causes the eyes to deviate downwards and warm water causes the eyes to deviate upwards
Caveats
- Brainstem encephalitis, deep metabolic coma and certain drugs may mimic brainstem death
- Drugs include recently administered anticonvulsants such as phenytoin and barbiturates. Like phenytoin, tricyclic overdose may cause bilateral vestibular failure, as might aminoglycoside vestibulotoxicity. Baclofen overdose can also mimic brain death
- Another caveat pertains to the trauma patient — ocular movements may be impaired if a blowout fracture has trapped the extraocular muscles
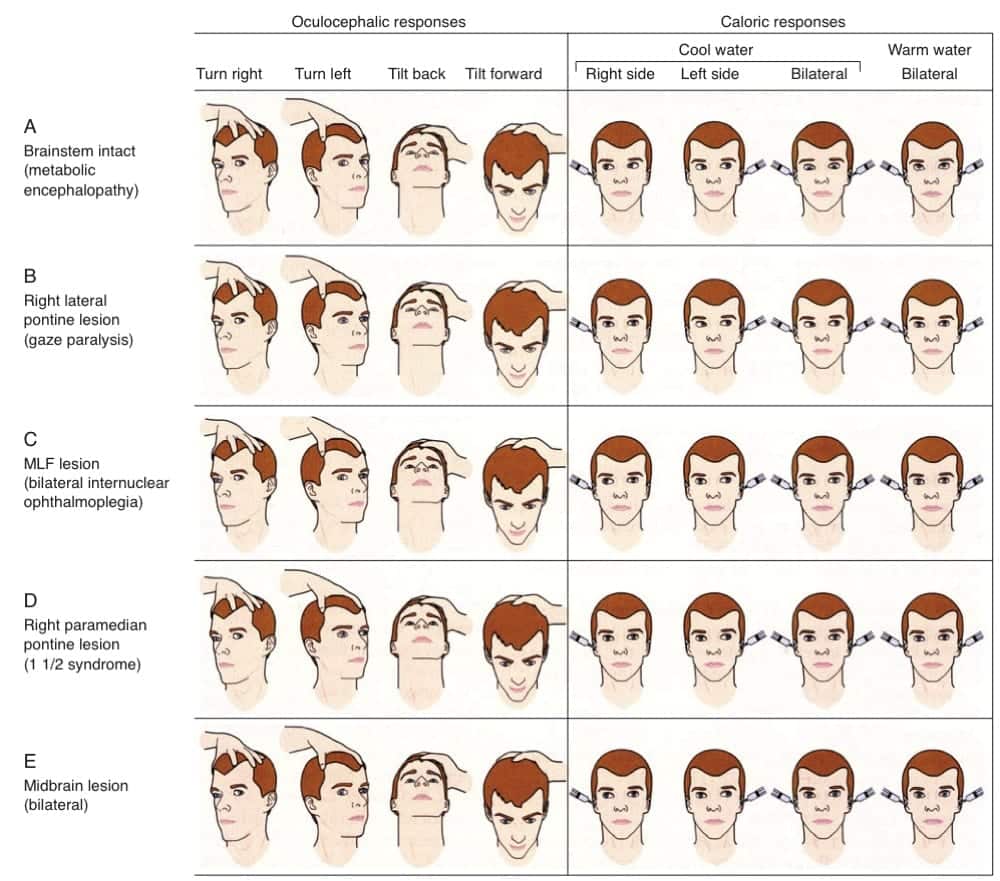
Typical findings for various lesions are shown in this graphic from Posner et al (2008):
SPONTANEOUS EYE MOVEMENTS
CORNEAL REFLEX
Corneal reflex is of limited use
- patients that chronically wear contact lenses may have diminished corneal reflexes
- loss of the corneal reflex is usually a late sign in coma
Assessment
- traditional method is to stroke the cornea with cotton wool
- corneal stimulation can also be performed by dropping a few drops of sterile saline onto the cornea from a height of 10 cm (less traumatic)
- reflex is present and intact if the patient blinks and eyes roll upwards
- afferent: CN5
- efferent: CN7 (blink) and CN3 (eye movement)
- indicates that the pons and midbrain are intact (the reflex pathway involves the trigeminal nerve, the spinal CN5 nucleus, the lateral brainstem tegmentum, and the CN3 and CN7 nuclei)
- If the eye turns upwards but the eyelid does not close there is a CN7 lesion (Bell’s phenomenon)
- If the eye does not turn upwards and the eyelid does not close there is a CN5 lesion
GAG AND COUGH REFLEXES
Gag reflex
- sensory = CN9, motor = CN10
- may be absent in normal people and those accustomed to an endotracheal tube
- best assessed using a laryngoscope and a tongue depressor in intubated patients, look for bilateral palatal elevation
Cough reflex
- mediated by CN10
- can be stimulated by a suction catheter down and endotracheal tube
MOTOR RESPONSES
Posturing can occur spontaneously or in response to a stimulus
- Abnormal flexion is decorticate posturing — adduction of arm, internal rotation of shoulder, pronation of forearm, flexion of wrist (lower limbs are extended); indicates a lesion above the brainstem
- Extension is decerebrate posturing — abduction of arm, external rotation of shoulder, supination of forearm, extension of wrist (lower limbs are extended); indicates a lesion extending to the midbrain or below
Assess for:
- tone
- clonus
- deep tendon reflexes
- plantar reflexes
- involuntary movements (such as subtle signs of seizures and myoclonus)
Look for asymmetry
SIGNS OF THE UNDERLYING CAUSE
- consider the neurological findings in light of the vital signs, evidence of trauma or shock, acute or chronic illness, and/or drug ingestion
- cranial scars, drains, ICP monitors and VP shunts
- neck stiffness
- track marks, drug paraphernalia and toxidromes
- infusions (e.g. sedatives, nimodipine, vasopressors)
- ventilator (evidence of spontaneous breaths?)
- Look in the fundi for papilloedema, diabetic or hypertensive retinopathy, or subhyaloid haemorrhage
FUNDOSCOPY
Important findings include:
- papilloedema —
optic disc swelling due to raised intracranial pressure. However, the absence of papilloedema does not rule out intracranial hypertension… - evidence of Terson syndrome —
vitreous, subhyaloid, or retinal bleeding in association with subarachnoid hemorrhage
VIDEO
Bedside demonstration and discussion of the examination of the unconscious patient by Peter T. Skaff, M.D., Neurologist with the Mercy Neurological Institute of Greater Sacramento:
References and Links
Introduction to ICU Series
Introduction to ICU Series Landing Page
DAY TO DAY ICU: FASTHUG, ICU Ward Round, Clinical Examination, Communication in a Crisis, Documenting the ward round in ICU, Human Factors
AIRWAY: Bag Valve Mask Ventilation, Oropharyngeal Airway, Nasopharyngeal Airway, Endotracheal Tube (ETT), Tracheostomy Tubes
BREATHING: Positive End Expiratory Pressure (PEEP), High Flow Nasal Prongs (HFNP), Intubation and Mechanical Ventilation, Mechanical Ventilation Overview, Non-invasive Ventilation (NIV)
CIRCULATION: Arrhythmias, Atrial Fibrillation, ICU after Cardiac Surgery, Pacing Modes, ECMO, Shock
CNS: Brain Death, Delirium in the ICU, Examination of the Unconscious Patient, External-ventricular Drain (EVD), Sedation in the ICU
GASTROINTESTINAL: Enteral Nutrition vs Parenteral Nutrition, Intolerance to EN, Prokinetics, Stress Ulcer Prophylaxis (SUP), Ileus
GENITOURINARY: Acute Kidney Injury (AKI), CRRT Indications
HAEMATOLOGICAL: Anaemia, Blood Products, Massive Transfusion Protocol (MTP)
INFECTIOUS DISEASE: Antimicrobial Stewardship, Antimicrobial Quick Reference, Central Line Associated Bacterial Infection (CLABSI), Handwashing in ICU, Neutropenic Sepsis, Nosocomial Infections, Sepsis Overview
SPECIAL GROUPS IN ICU: Early Management of the Critically Ill Child, Paediatric Formulas, Paediatric Vital Signs, Pregnancy and ICU, Obesity, Elderly
FLUIDS AND ELECTROLYTES: Albumin vs 0.9% Saline, Assessing Fluid Status, Electrolyte Abnormalities, Hypertonic Saline
PHARMACOLOGY: Drug Infusion Doses, Summary of Vasopressors, Prokinetics, Steroid Conversion, GI Drug Absorption in Critical Illness
PROCEDURES: Arterial line, CVC, Intercostal Catheter (ICC), Intraosseous Needle, Underwater seal drain, Naso- and Orogastric Tubes (NGT/OGT), Rapid Infusion Catheter (RIC)
INVESTIGATIONS: ABG Interpretation, Echo in ICU, CXR in ICU, Routine daily CXR, FBC, TEG/ROTEM, US in Critical Care
ICU MONITORING: NIBP vs Arterial line, Arterial Line Pressure Transduction, Cardiac Output, Central Venous Pressure (CVP), CO2 / Capnography, Pulmonary Artery Catheter (PAC / Swan-Ganz), Pulse Oximeter
CCC Neurocritical Care Series
Emergencies: Brain Herniation, Eclampsia, Elevated ICP, Status Epilepticus, Status Epilepticus in Paeds
DDx: Acute Non-Traumatic Weakness, Bulbar Dysfunction, Coma, Coma-like Syndromes, Delayed Awakening, Hearing Loss in ICU, ICU acquired Weakness, Post-Op Confusion, Pseudocoma, Pupillary Abnormalities
Neurology: Anti-NMDA Encephalitis, Basilar Artery Occlusion, Central Diabetes Insipidus, Cerebral Oedema, Cerebral Venous Sinus Thrombosis, Cervical (Carotid / Vertebral) Artery Dissections, Delirium, GBS vs CIP, GBS vs MG vs MND, Guillain-Barre Syndrome, Horner’s Syndrome, Hypoxic Brain Injury, Intracerebral Haemorrhage (ICH), Myasthenia Gravis, Non-convulsive Status Epilepticus, Post-Hypoxic Myoclonus, PRES, Stroke Thrombolysis, Transverse Myelitis, Watershed Infarcts, Wernicke’s Encephalopathy
Neurosurgery: Cerebral Salt Wasting, Decompressive Craniectomy, Decompressive Craniectomy for Malignant MCA Syndrome, Intracerebral Haemorrhage (ICH)
— SCI: Anatomy and Syndromes, Acute Traumatic Spinal Cord Injury, C-Spine Assessment, C-Spine Fractures, Spinal Cord Infarction, Syndomes,
— SAH: Acute management, Coiling vs Clipping, Complications, Grading Systems, Literature Summaries, ICU Management, Monitoring, Overview, Prognostication, Vasospasm
— TBI: Assessment, Base of skull fracture, Brain Impact Apnoea, Cerebral Perfusion Pressure (CPP), DI in TBI, Elevated ICP, Limitations of CT, Lund Concept, Management, Moderate Head Injury, Monitoring, Overview, Paediatric TBI, Polyuria incl. CSW, Prognosis, Seizures, Temperature
ID in NeuroCrit. Care: Aseptic Meningitis, Bacterial Meningitis, Botulism, Cryptococcosis, Encephalitis, HSV Encephalitis, Meningococcaemia, Spinal Epidural Abscess
Equipment/Investigations: BIS Monitoring, Codman ICP Monitor, Continuous EEG, CSF Analysis, CT Head, CT Head Interpretation, EEG, Extradural ICP Monitors, External Ventricular Drain (EVD), Evoked Potentials, Jugular Bulb Oxygen Saturation, MRI Head, MRI and the Critically Ill, Train of Four (TOF), Transcranial Doppler
Pharmacology: Desmopressin, Hypertonic Saline, Levetiracetam (Keppra), Mannitol, Midazolam, Sedation in ICU, Thiopentone
MISC: Brainstem Rules of 4, Cognitive Impairment in Critically Ill, Eye Movements in Coma, Examination of the Unconscious Patient, Glasgow Coma Scale (GCS), Hiccoughs, Myopathy vs Neuropathy, Neurology Literature Summaries, NSx Literature Summaries, Occulocephalic and occulovestibular reflexes, Prognosis after Cardiac Arrest, SIADH vs Cerebral Salt Wasting, Sleep in ICU
LITFL
- Neurological Mind-boggler 007 — Eye Movements, Coma And Pseudocoma (2010)
- CCC — Coma Hot Case
- CCC — Brain Death Hot Case
Journal articles
- Walker MC, O’Brien MD. Neurological examination of the unconscious patient. J R Soc Med. 1999 Jul;92(7):353-5. PMC1297287.
Textbooks
- Posner JB, Saper CB, Schiff N, Plum F. Plum and Posner’s Diagnosis of Stupor and Coma 4e Oxford university Press, 2009.

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

Hi Chris
Thanks for all the helpful information. How can this information be used to prognostic a patient. Say the situation yesterday. 25mins CPR, unknown down time, initial rhythm asystole. Massive STEMI on ECG and cath lab asks “if its worth doing a cath because of likely poor neuro outcome.” Patient had spont breathing, pupillary reflex and slight movement of arms. I don’t have the experience to understand how comatose patients with this type of exam will fair. So we got ICU down and assessed him and they felt he might make meaningful recovery. How can I arm myself better to prevent a delay to the cath in the future. Thanks
Hi
There is a separate page on prognosis after cardiac arrest:
https://litfl.com/prognosis-after-cardiac-arrest/
I can understand the skepticism given asystole typically has poor outcomes, but things change once ROSC is achieved! From what you describe there were no indicators of definitive poor neurological outcome. In general, neuroprognostication cannot be definitively made immediately after ROSC – usually need to wait until 72 hours after completion of targeted temperature management (if used for asystole, or time of arrest).
Exceptions are:
1. patients with myoclonus status in the first 24 hours after admission and a bilateral absence of N20-peak on median nerve somatosensory evoked potentials (SSEP)
2. patients who became brain dead due to cerebral herniation
3. other grounds for early palliation (e.g. terminal cancer, previously stated patient wishes)
Timing of going to cath lab in such circumstances is often problematic. Some clinicians want to wait for patients to show “wake up” (show evidence of likely meaningful recovery), however, this approach risks the patient re-arresting in the days that follow and a poor outcome becoming a self-fulfilling prophecy.
In general, my approach is to advocate for early cath lab when there is a likely STEMI and indeterminate neurology, unless there is high likelihood of the above exceptions.
Cheers
Chris
Thanks for the information. Your article on prognostication in cardiac arrest was very helpful. Thank you again