CSF analysis
OVERVIEW
- CSF = cerebrospinal fluid
THINGS TO PUT ON THE FORM
- gram stain
- microscopy
- culture
- xanthochromia
- WCC
- RCC
- protein
- oligoclonal bands
- extended culture
- cryptoccal antigen and Indian ink stain
- ZN stain for acid fast bacilli
- PCR for enterovirus and HSV
- cytology
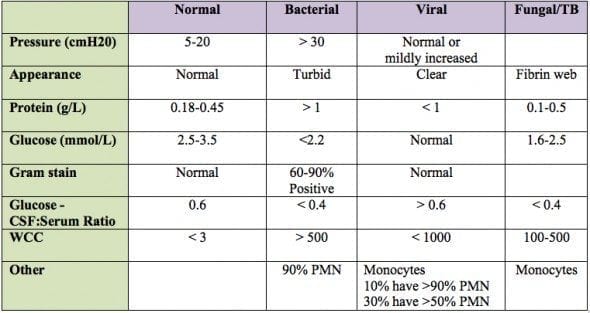
APPEARANCE
- normally clear
- turbid with infection
- blood stained with SAH and traumatic taps
- yellow with xanthochromia (this takes 6-12 hours to develop after blood enters CSF)
WCC
- normally scant monocytes
- in traumatic tap classically taught to expect 1 WCC : 500 RCC (if normal in peripheral cell counts) but this is not reliable
- polymorphonuclear leukocytosis: bacterial infection
- lymphocytosis: viral, TB, cryptococcal and listerial infections
- mixed lymphocytosis/monocytosis in GBS and status epilepticus
RCC
- increased in traumatic tap and SAH
PROTEIN
- increased in infection: Tb > bacterial > viral
- increased in GBS, vasculitis and sarcoidosis
- oligoclonal bands in multiple sclerosis
- increased in CNS inflammation (including CSF drains and blood in CSF)
GLUCOSE
- normally at least 75% serum glucose
- less than half serum in infections (bacterial, Tb and fungal infections) and vasculitis and sarcoidosis
OTHER FINDINGS
- xanthochromic index with spectrophotometry (in SAH)
- extended culture (Listeria, Cryptococcus)
- India Ink stain for cryptococcus
- ZN stain for acid fast bacilli
- PCR for enterovirus and HSV
- cytology
Meningitis
- Infective
- Bacterial
- Aseptic – Viral, TB, Fungi, Parasites
- Non-infective
- Malignancy
- Auto-immune
Age-related Causes of Meningitis
- Bacterial:
- Neonatal (<3/12)
- Gram negative (E coli)(Pseudomonas), Listeria, Group B strep, Coag –ve staphylococcus
- 3/12 to 15 years
- Neiserria meningitidis, Pneumococcus (strep pneumonia), Haemophilus pneumonia
- Adult > 15 years
- N meningitidis, s. pneumonia, listeria, klebsiella, s. aureus
- Elderly
- Gram negatives predominate
- Immunocompromised
- Complement deficiency – Neiserria
- Humoral or asplenic – Neiserria, enterovirus
- Sickle cell disease – Capsulated organisms
- Neonatal (<3/12)
- Aseptic meningitis (Generally accepted as mainly viral meningitis)
- Lymphocytosis, variable protein elevation and normal glucose
- Viral
- Echovirus, Enterovirus, Mumps
- HSV 1 + 2, CMV, VZV, EBV
- Other
- TB, Nocardia, Leptospira, Treponema
- Fungi, rickettsia, parasites
- Malignancy, auto-immune
Specific Risk Factors
- Pneumococcus: (40%) – Otitis media, head injury, pneumonia, immunocompromised
- N meningitidis: (30%) – Children and adolescents
- Staphylococcus: Penetrating skull injury, ear or neuro operations
- Fungal: HIV and organ transplant
- Listeria: Extremes of age
- H Influenzae: (3%) – Head trauma with CSF leak, otitis, sinusitis, anatomical defects such as dermal sinus tracts
- Anaerobes: Consider brain abscess, elderly
References and Links
CCC Neurocritical Care Series
Emergencies: Brain Herniation, Eclampsia, Elevated ICP, Status Epilepticus, Status Epilepticus in Paeds
DDx: Acute Non-Traumatic Weakness, Bulbar Dysfunction, Coma, Coma-like Syndromes, Delayed Awakening, Hearing Loss in ICU, ICU acquired Weakness, Post-Op Confusion, Pseudocoma, Pupillary Abnormalities
Neurology: Anti-NMDA Encephalitis, Basilar Artery Occlusion, Central Diabetes Insipidus, Cerebral Oedema, Cerebral Venous Sinus Thrombosis, Cervical (Carotid / Vertebral) Artery Dissections, Delirium, GBS vs CIP, GBS vs MG vs MND, Guillain-Barre Syndrome, Horner’s Syndrome, Hypoxic Brain Injury, Intracerebral Haemorrhage (ICH), Myasthenia Gravis, Non-convulsive Status Epilepticus, Post-Hypoxic Myoclonus, PRES, Stroke Thrombolysis, Transverse Myelitis, Watershed Infarcts, Wernicke’s Encephalopathy
Neurosurgery: Cerebral Salt Wasting, Decompressive Craniectomy, Decompressive Craniectomy for Malignant MCA Syndrome, Intracerebral Haemorrhage (ICH)
— SCI: Anatomy and Syndromes, Acute Traumatic Spinal Cord Injury, C-Spine Assessment, C-Spine Fractures, Spinal Cord Infarction, Syndomes,
— SAH: Acute management, Coiling vs Clipping, Complications, Grading Systems, Literature Summaries, ICU Management, Monitoring, Overview, Prognostication, Vasospasm
— TBI: Assessment, Base of skull fracture, Brain Impact Apnoea, Cerebral Perfusion Pressure (CPP), DI in TBI, Elevated ICP, Limitations of CT, Lund Concept, Management, Moderate Head Injury, Monitoring, Overview, Paediatric TBI, Polyuria incl. CSW, Prognosis, Seizures, Temperature
ID in NeuroCrit. Care: Aseptic Meningitis, Bacterial Meningitis, Botulism, Cryptococcosis, Encephalitis, HSV Encephalitis, Meningococcaemia, Spinal Epidural Abscess
Equipment/Investigations: BIS Monitoring, Codman ICP Monitor, Continuous EEG, CSF Analysis, CT Head, CT Head Interpretation, EEG, Extradural ICP Monitors, External Ventricular Drain (EVD), Evoked Potentials, Jugular Bulb Oxygen Saturation, MRI Head, MRI and the Critically Ill, Train of Four (TOF), Transcranial Doppler
Pharmacology: Desmopressin, Hypertonic Saline, Levetiracetam (Keppra), Mannitol, Midazolam, Sedation in ICU, Thiopentone
MISC: Brainstem Rules of 4, Cognitive Impairment in Critically Ill, Eye Movements in Coma, Examination of the Unconscious Patient, Glasgow Coma Scale (GCS), Hiccoughs, Myopathy vs Neuropathy, Neurology Literature Summaries, NSx Literature Summaries, Occulocephalic and occulovestibular reflexes, Prognosis after Cardiac Arrest, SIADH vs Cerebral Salt Wasting, Sleep in ICU
Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

Hi Chris,
In the table, protein in TB CSF appears to be wrong. It should be 1-5, not 0.1-0.5 gm/L
its not. the units are in g, so 0.1 g = 1 mg.