Oculocephalic and oculovestibular reflexes
OVERVIEW
Oculocephalic and oculovestibular reflexes are primarily used to determine whether a patient’s brainstem is intact (e.g. coma or brain death assessment)
OCULOCEPHALIC REFLEX
Oculocephalic reflex:
- ensure the C-spine is cleared.
- the patient’s eyes are held open.
- the head is briskly turned from side to side with the head held briefly at the end of each turn.
- a positive response occurs when the eyes rotate to the opposite side to the direction of head rotation, thus indicating that the brainstem (CN3,6,8) is intact.
- a similar result is seen when the head is flexed and extended — a positive result is downward deviation of the eyes during extension, and upward deviation during flexion (the eyelids, if closed, may also open as part of the ‘doll’s head phenomenon’). These vertical responses indicates that the brainstem (CN3,4,8) is intact.
- The eyes should gradually return to the mid-position in a smooth, conjugate movement if the brainstem is intact.
Patients with metabolic coma (e.g. hepatic failure) may have exaggerated, brisk oculocephalic reflexes.
OCULOVESTIBULAR REFLEX
Oculovestibular reflex (caloric stimulation):
- the head is elevated to 30 degrees above horizontal so that the lateral semicircular canal is vertical, and so that stimulation with generate a maximal response.
- check that the tympanum is intact and that the external ear canal is clear — C-spine clearance is not necessary.
- introduce iced water into the external ear canal through a small catheter until one of the following occurs:
- nystagmus (in the intact brainstem the slow phase is towards the irrigated ear)
- ocular deviation
- 200mL of iced water has been instilled.
- allow 5 minutes between testing ears to allow re-equilibration of the oculovestibular system.
- as consciousness is lost, the fast component (towards the non-irrigated ear) is lost and the slow component deviates the eye in the direction of the irrigated ear.
Vertical oculovestibular eye responses can be assessed by irrigating both ears simultaneously.
- If the brainstem is intact, cold water causes the eyes to deviate downwards and warm water causes the eyes to deviate upwards.
The positive brainstem responses described above are those seen in a comatose patient with an intact brainstem.
TYPICAL FINDINGS
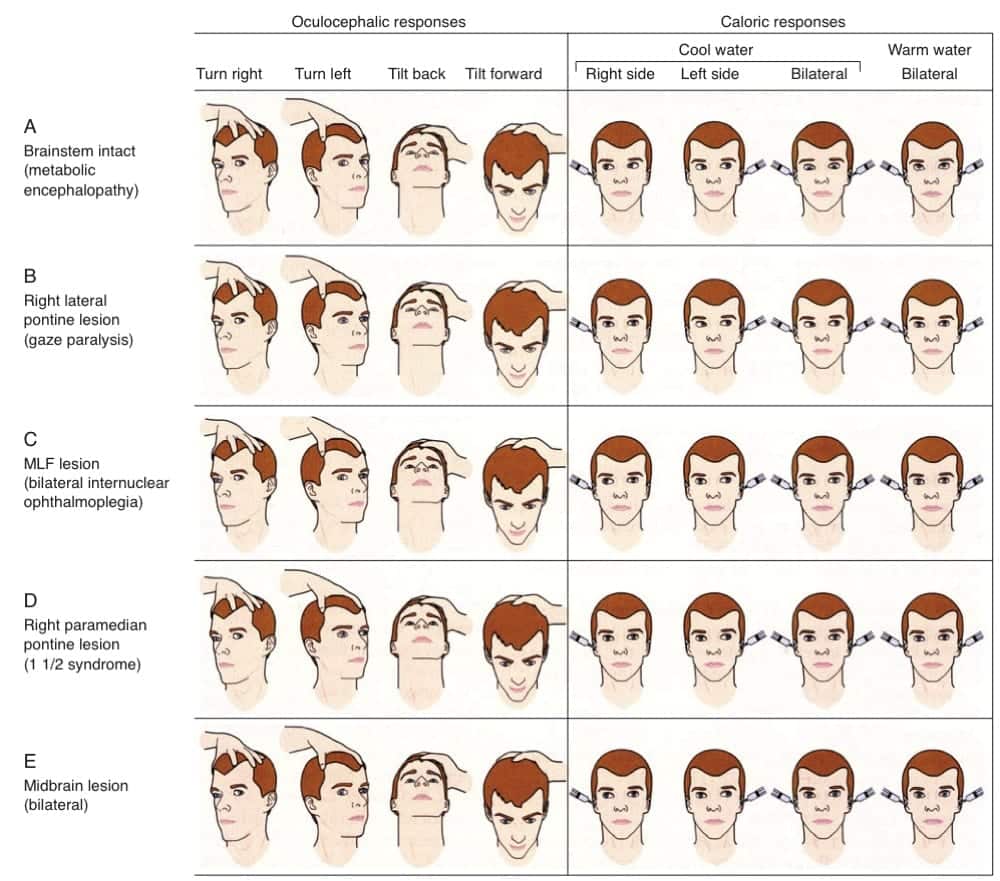
Typical findings for various lesions are shown in this graphic from Posner et al (2008):
References and Links
CCC Neurocritical Care Series
Emergencies: Brain Herniation, Eclampsia, Elevated ICP, Status Epilepticus, Status Epilepticus in Paeds
DDx: Acute Non-Traumatic Weakness, Bulbar Dysfunction, Coma, Coma-like Syndromes, Delayed Awakening, Hearing Loss in ICU, ICU acquired Weakness, Post-Op Confusion, Pseudocoma, Pupillary Abnormalities
Neurology: Anti-NMDA Encephalitis, Basilar Artery Occlusion, Central Diabetes Insipidus, Cerebral Oedema, Cerebral Venous Sinus Thrombosis, Cervical (Carotid / Vertebral) Artery Dissections, Delirium, GBS vs CIP, GBS vs MG vs MND, Guillain-Barre Syndrome, Horner’s Syndrome, Hypoxic Brain Injury, Intracerebral Haemorrhage (ICH), Myasthenia Gravis, Non-convulsive Status Epilepticus, Post-Hypoxic Myoclonus, PRES, Stroke Thrombolysis, Transverse Myelitis, Watershed Infarcts, Wernicke’s Encephalopathy
Neurosurgery: Cerebral Salt Wasting, Decompressive Craniectomy, Decompressive Craniectomy for Malignant MCA Syndrome, Intracerebral Haemorrhage (ICH)
— SCI: Anatomy and Syndromes, Acute Traumatic Spinal Cord Injury, C-Spine Assessment, C-Spine Fractures, Spinal Cord Infarction, Syndomes,
— SAH: Acute management, Coiling vs Clipping, Complications, Grading Systems, Literature Summaries, ICU Management, Monitoring, Overview, Prognostication, Vasospasm
— TBI: Assessment, Base of skull fracture, Brain Impact Apnoea, Cerebral Perfusion Pressure (CPP), DI in TBI, Elevated ICP, Limitations of CT, Lund Concept, Management, Moderate Head Injury, Monitoring, Overview, Paediatric TBI, Polyuria incl. CSW, Prognosis, Seizures, Temperature
ID in NeuroCrit. Care: Aseptic Meningitis, Bacterial Meningitis, Botulism, Cryptococcosis, Encephalitis, HSV Encephalitis, Meningococcaemia, Spinal Epidural Abscess
Equipment/Investigations: BIS Monitoring, Codman ICP Monitor, Continuous EEG, CSF Analysis, CT Head, CT Head Interpretation, EEG, Extradural ICP Monitors, External Ventricular Drain (EVD), Evoked Potentials, Jugular Bulb Oxygen Saturation, MRI Head, MRI and the Critically Ill, Train of Four (TOF), Transcranial Doppler
Pharmacology: Desmopressin, Hypertonic Saline, Levetiracetam (Keppra), Mannitol, Midazolam, Sedation in ICU, Thiopentone
MISC: Brainstem Rules of 4, Cognitive Impairment in Critically Ill, Eye Movements in Coma, Examination of the Unconscious Patient, Glasgow Coma Scale (GCS), Hiccoughs, Myopathy vs Neuropathy, Neurology Literature Summaries, NSx Literature Summaries, Occulocephalic and occulovestibular reflexes, Prognosis after Cardiac Arrest, SIADH vs Cerebral Salt Wasting, Sleep in ICU
- Posner JB, Saper CB, Schiff N, Plum F. Plum and Posner’s Diagnosis of Stupor and Coma 4e Oxford university Press, 2009.
Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
