Intercostal Catheter (Chest Drain)
OVERVIEW
- tube inserted into pleural space to allow drainage of contents
USES
- drainage of air/fluid from pleural space
- pleural lavage (e.g. rewarming in severe hypothermia)
METHOD OF INSERTION AND/OR USE
Anatomy
- insertion should take place on same side of haemothorax (ie. left)
- landmarks = “triangle of safety”: anterior to mid axillary line, posterior to pectoral groove, above 5th intercostal space
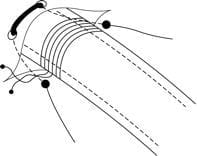
- layers that must be breached (superficial to deep) = skin, subcutaneous tissue, intercostal muscles, parietal pleura
- awareness of the intercostal bundle sitting on the inferior aspect of the ribs
Equipment
- sterile clothing (gloves, gown, hat, mask, facial shield)
- chlorhexidine in 80% alcohol
- sterile drapes
- lignocaine 1%
- 22G long needle
- scalpel
- curved forceps
- chest drain (>24 French for blood)
- suture material
- underwater seal drain
- dressing
Technique
- explain procedure, obtain consent, sterile environment with equipment ready, skilled assistant, adequate analgesia, adequate resuscitation equipment and recovery facilities
- check coagulation profile, Hb, platelet number -> transfuse accordingly
- in this patient it will be important to check urea as this will probably be elevated and will cause platelet dysfunction
- position patient (supine or 30 degrees head up) with arm abducted & elbow flexed
- sterile preparation of area
- identify rib spaces (4th to 7th) on left and anterior – mid axillary line
- skin infiltration with lignocaine 1%
- infiltrate down to parietal pleura (ensuring needle travels over the top of the chosen rib to protect neurovascular bundle)
- continuous aspiration of needle should reveal blood once in the pleural space
- make an incision following line of ribs with scalpel (1 to 2cm long)
- blunt dissection with finger or blunt forceps (this will ensure adherent lung is moved from insertion site)
- once parietal pleura breeched there should be a rush of blood
- dilate with finger
- load chest drain onto curved forceps (orientated towards the apex)
- use forceps to allow the clamped drain to follow the true lumen that has been created
- insert drain until an adequate length is within the pleural cavity (will depend of patient habitus)
- suture in place and dress with a sterile dressing
- connect to underwater seal drain (connections should be stable and easy to attach in a sterile manner)
- CXR should be formed to check adequate positioning and detect complications
OTHER INFORMATION
- connected to underwater seal drain (see separate CCC entry)
COMPLICATIONS
Insertion
- pain
- damage to local structures
- pulmonary injury and bronchopleural fistula
- bleeding
- insertion into a vascular structure (pulmonary artery or left ventricle)
- infection
Use
- tube blockage
- tube displacement
- dislodgement
- infection
- misuse of drainage system leading to introduction of air or fluid into pleural cavity
Removal
- recurrence of underlying condition
- wound dehiscence
- scarring
VIDEOS
Insertion of intercostal catheter
Removal of intercostal catheter
Insertion of pigtail catheter using obturator and Seldinger technique
References and Links
Introduction to ICU Series
Introduction to ICU Series Landing Page
DAY TO DAY ICU: FASTHUG, ICU Ward Round, Clinical Examination, Communication in a Crisis, Documenting the ward round in ICU, Human Factors
AIRWAY: Bag Valve Mask Ventilation, Oropharyngeal Airway, Nasopharyngeal Airway, Endotracheal Tube (ETT), Tracheostomy Tubes
BREATHING: Positive End Expiratory Pressure (PEEP), High Flow Nasal Prongs (HFNP), Intubation and Mechanical Ventilation, Mechanical Ventilation Overview, Non-invasive Ventilation (NIV)
CIRCULATION: Arrhythmias, Atrial Fibrillation, ICU after Cardiac Surgery, Pacing Modes, ECMO, Shock
CNS: Brain Death, Delirium in the ICU, Examination of the Unconscious Patient, External-ventricular Drain (EVD), Sedation in the ICU
GASTROINTESTINAL: Enteral Nutrition vs Parenteral Nutrition, Intolerance to EN, Prokinetics, Stress Ulcer Prophylaxis (SUP), Ileus
GENITOURINARY: Acute Kidney Injury (AKI), CRRT Indications
HAEMATOLOGICAL: Anaemia, Blood Products, Massive Transfusion Protocol (MTP)
INFECTIOUS DISEASE: Antimicrobial Stewardship, Antimicrobial Quick Reference, Central Line Associated Bacterial Infection (CLABSI), Handwashing in ICU, Neutropenic Sepsis, Nosocomial Infections, Sepsis Overview
SPECIAL GROUPS IN ICU: Early Management of the Critically Ill Child, Paediatric Formulas, Paediatric Vital Signs, Pregnancy and ICU, Obesity, Elderly
FLUIDS AND ELECTROLYTES: Albumin vs 0.9% Saline, Assessing Fluid Status, Electrolyte Abnormalities, Hypertonic Saline
PHARMACOLOGY: Drug Infusion Doses, Summary of Vasopressors, Prokinetics, Steroid Conversion, GI Drug Absorption in Critical Illness
PROCEDURES: Arterial line, CVC, Intercostal Catheter (ICC), Intraosseous Needle, Underwater seal drain, Naso- and Orogastric Tubes (NGT/OGT), Rapid Infusion Catheter (RIC)
INVESTIGATIONS: ABG Interpretation, Echo in ICU, CXR in ICU, Routine daily CXR, FBC, TEG/ROTEM, US in Critical Care
ICU MONITORING: NIBP vs Arterial line, Arterial Line Pressure Transduction, Cardiac Output, Central Venous Pressure (CVP), CO2 / Capnography, Pulmonary Artery Catheter (PAC / Swan-Ganz), Pulse Oximeter

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
