Thromboelastogram (TEG)
Reviewed and revised by Hamish Lala and Chris Nickson
OVERVIEW
Thromboelastography (TEG) is a viscoelastic hemostatic assay that measures the global viscoelastic properties of whole blood clot formation under low shear stress
- TEG shows the interaction of platelets with the coagulation cascade (aggregation, clot strengthening, fibrin cross-linking and fibrinolysis)
- does not necessarily correlate with blood tests such as INR, APTT and platelet count (which are often poorer predictors of bleeding and thrombosis)
- This page describes TEG® predominantly, ROTEM® is the alternative viscoelastic hemostatic assay that is widely available commercially
METHOD
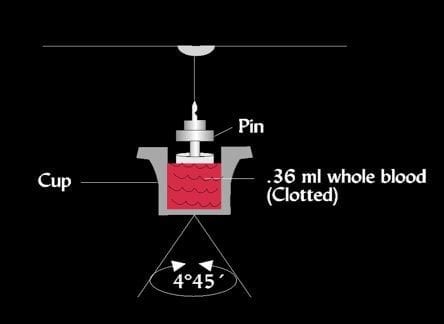
- TEG® measures the physical properties of the clot in whole blood via a pin suspended in a cup (heated to 37C) from a torsion wire connected with a mechanical-electrical transducer
- The elasticity and strength of the developing clot changes the rotation of the pin, which is converted into electrical signals that a computer uses to create graphical and numerical output
- point of care test (quick, takes around 30min)
- can be repeated easily and compared and contrasted
- requires calibration 2-3 times daily
- should be performed by trained personnel
- susceptible to technical variations
- kaolin and more recently kaolin + tissue factor (TF) (RapidTEG®) are used as activators, NATEM (TEG® using native whole blood) is slower
- other tests are available including functional fibrinogen, a measure of fibrin-based clot function, and Multiplate which evaluates platelet function
TEG6s (Haemonetics)
- This newer machine no longer uses the ‘pin-in-cup’ technique (as did its TEG5000 predecessor)
- It uses ‘resonance’ where blood is exposed to a fixed vibration frequency range and the detector measures the vertical motion of blood meniscus under LED illumination and transforms that movement into tracing of clot dynamics
- With pre-prepared cartridges, there is no longer any pipetting required!
USE
Indications
- prediction of need for transfusion (maximum amplitude (MA) is a useful predictor in trauma)
- guide transfusion strategy
Studies show cost-effectiveness and reduction in blood products in:
- liver transplantation
- cardiac surgery
Maybe useful in:
- trauma (reduction in blood product use and mortality in cohort studies)
- obstetrics (some data to show that it may decrease transfusion rates; this is controversial)
- early detection of dilutional coagulopathy
Hard to interpret in certain situations:
- low molecular weight heparin (LMWH)
- aspirin
- post cardiac bypass
- fibrinolysis
- hypercoagulability
NORMAL TEG
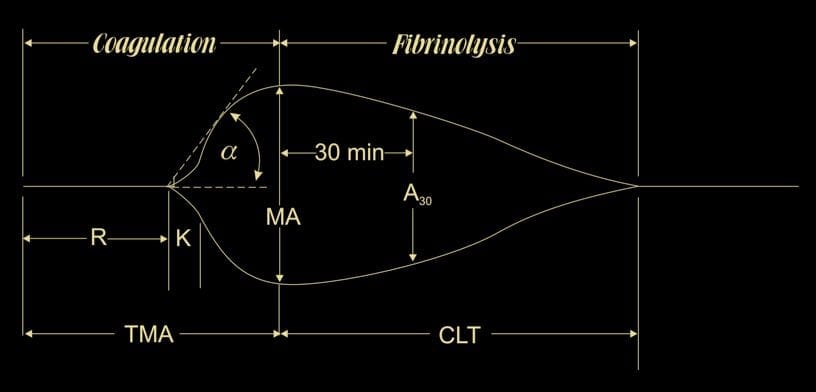
Specific parameters represent the 3 phases of the cell-based model of haemostasis: initiation, amplification, and propagation
- R value = reaction time (s)
- time of latency from start of test to initial fibrin formation (amplitude of 2mm)
- initiation phase
- dependent on clotting factors
- K = kinetics (s)
- time taken to achieve a certain level of clot strength (amplitude of 20mm)
- amplification phase
- dependent on fibrinogen
- alpha = angle (slope of line between R and K)
- measures the speed at which fibrin build up and cross-linking takes place, hence assesses the rate of clot formation
- “thrombin burst” / propagation phase
- dependent on fibrinogen
- TMA = time to maximum amplitude(s)
- MA = maximum amplitude (mm)
- represents the ultimate strength of the fibrin clot; i.e. overall stability of the clot
- dependent on platelets (80%) and fibrin (20%) interacting via GPIIb/IIIa
- A30 or LY30 = amplitude at 30 minutes
- percentage decrease in amplitude at 30 minutes post-MA
- fibrinolysis phase
- CLT = clot lysis time (s)
Approximate normal values (kaolin activated TEG, values differ if native blood used, and between types of assay)
- R: 4-8 min
- K: 1-4 min
- α-Angle: 47-74°
- MA: 55-73mm
- LY 30%: 0-8%
Corresponding terminology for ROTEM
| ROTEM | TEG |
| Clotting time (CT) | R value (reaction time) |
| α angle and clot formation time (CFT) | K value and α angle |
| Maximum clot firmness (MCF) | Maximum amplitude (MA) |
| Clot lysis (CL) | LY30 |
IMPORTANT PATTERNS
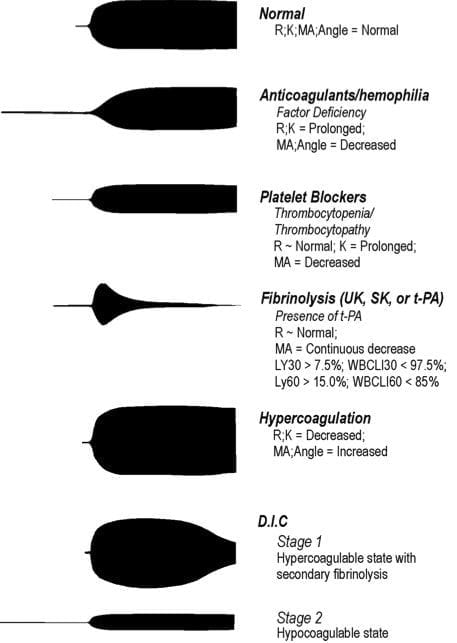
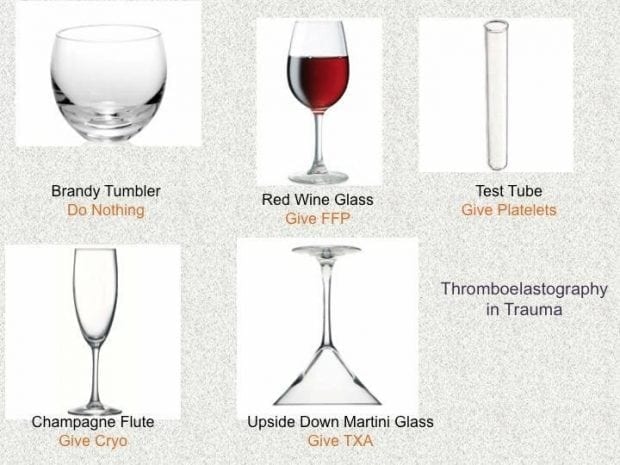
TEG AS A GUIDE TO TREATMENT
- Increased R time => FFP
- Decreased alpha angle => cryoprecipitate
- Decreased MA => platelets (consider DDAVP)
- Fibrinolysis => tranexamic acid (or aprotinin or aminocaproic acid)
Or use this handy guide (-:
TEG® VERSUS ROTEM®
Comparison
- Two commercial types of viscoelastic tests are available: thromboelastography =TEG® (developed in 1948, now produced in the USA) and rotational thromboelastogram = ROTEM® (from Germany)
- differences in diagnostic nomenclature for identical parameters between the two
- TEG® operates by moving a cup in a limited arc (±4°45′ every 5s) filled with sample that engages a pin/wire transduction system as clot formation occur
- ROTEM® has an immobile cup wherein the pin/wire transduction system slowly oscillates (±4°45′every 6s)
- results are not directly comparable as different coagulation activators are used
- ROTEM® is more resistant to mechanical shock, which may be an advantage in the clinical setting
Equivalent variables for ROTEM®
- Clotting time (CT) = R value (reaction time)
- α angle and clot formation time (CFT) = K value and α angle
- Maximum clot firmness (MCF) = Maximum amplitude (MA)
- Clot lysis (CL) = LY30
COMPARISON WITH PLASMA CLOTTING TESTS
Pros of viscoelastic hemostatic assays
- assessment of global haemostatic potential provides more information than time to fibrin formation
- can readily differentiate a coagulopathy due to low fibrinogen from one due to thrombocytopenia
- point-of-care (POC) device with rapid turnaround times so that many results available within 5–10 min of starting the test
Cons of viscoelastic hemostatic assays
- variable availability and user familiarity
- marked inter-operator variability and poor precision
- UK NEQAS data suggests coefficients of variance ranging from 7.1% to 39.9% for TEG® and 7.0% to 83.6% for ROTEM®
- may require specialist staff to perform
EVIDENCE
- Cochrane review (2015)of the use of TEG and ROTEM in traumatic bleeding advised that they should be used for research only, due to a lack of evidence for the accuracy of the assays.
References and Links
Introduction to ICU Series
Introduction to ICU Series Landing Page
DAY TO DAY ICU: FASTHUG, ICU Ward Round, Clinical Examination, Communication in a Crisis, Documenting the ward round in ICU, Human Factors
AIRWAY: Bag Valve Mask Ventilation, Oropharyngeal Airway, Nasopharyngeal Airway, Endotracheal Tube (ETT), Tracheostomy Tubes
BREATHING: Positive End Expiratory Pressure (PEEP), High Flow Nasal Prongs (HFNP), Intubation and Mechanical Ventilation, Mechanical Ventilation Overview, Non-invasive Ventilation (NIV)
CIRCULATION: Arrhythmias, Atrial Fibrillation, ICU after Cardiac Surgery, Pacing Modes, ECMO, Shock
CNS: Brain Death, Delirium in the ICU, Examination of the Unconscious Patient, External-ventricular Drain (EVD), Sedation in the ICU
GASTROINTESTINAL: Enteral Nutrition vs Parenteral Nutrition, Intolerance to EN, Prokinetics, Stress Ulcer Prophylaxis (SUP), Ileus
GENITOURINARY: Acute Kidney Injury (AKI), CRRT Indications
HAEMATOLOGICAL: Anaemia, Blood Products, Massive Transfusion Protocol (MTP)
INFECTIOUS DISEASE: Antimicrobial Stewardship, Antimicrobial Quick Reference, Central Line Associated Bacterial Infection (CLABSI), Handwashing in ICU, Neutropenic Sepsis, Nosocomial Infections, Sepsis Overview
SPECIAL GROUPS IN ICU: Early Management of the Critically Ill Child, Paediatric Formulas, Paediatric Vital Signs, Pregnancy and ICU, Obesity, Elderly
FLUIDS AND ELECTROLYTES: Albumin vs 0.9% Saline, Assessing Fluid Status, Electrolyte Abnormalities, Hypertonic Saline
PHARMACOLOGY: Drug Infusion Doses, Summary of Vasopressors, Prokinetics, Steroid Conversion, GI Drug Absorption in Critical Illness
PROCEDURES: Arterial line, CVC, Intercostal Catheter (ICC), Intraosseous Needle, Underwater seal drain, Naso- and Orogastric Tubes (NGT/OGT), Rapid Infusion Catheter (RIC)
INVESTIGATIONS: ABG Interpretation, Echo in ICU, CXR in ICU, Routine daily CXR, FBC, TEG/ROTEM, US in Critical Care
ICU MONITORING: NIBP vs Arterial line, Arterial Line Pressure Transduction, Cardiac Output, Central Venous Pressure (CVP), CO2 / Capnography, Pulmonary Artery Catheter (PAC / Swan-Ganz), Pulse Oximeter
CCC Transfusion Series
Blood Products: Cryoprecipitate, Fresh Frozen Plasma (FFP), Platelets, Red Cells (RBCs)
>>> Factor Concentrates: Prothrombinex, Factor VIIa, Fibrinogen Concentrate
Reversal Agents:
>>> Rivaroxaban / Apixaban / Enoxaparin: Andexanet Alfa, Rivaroxaban and Bleeding
>>> Dabigatran: Idarucuzimab, Dabigatran and bleeding
>>> Heparin: Protamine
>>> Warfarin: Vitamin K, FFP, PTx, Warfarin Refersal, Warfarin Toxicity
Testing: Coagulation Studies, TEG / ROTEM (Thromboelastography), Platelet function assays
Conditions: Acute Coagulopathy of Trauma, Disseminated Intravascular Coagulation (DIC), Massive Blood Loss
General Topics: Blood Bank, Blood Conservation Strategies, Blood Product Compatibilities, Blood Transfusion Risks, Massive Transfusion Protocol (MTP), Modifications to Blood Components, Procedures and Coagulopathy, Storage Lesions, TRALI, Transfusion Literature, Transfusion Reactions
Journal articles
- Afshari A, Wikkelsø A, Brok J, Møller AM, Wetterslev J. Thrombelastography (TEG) or thromboelastometry (ROTEM) to monitor haemotherapy versus usual care in patients with massive transfusion. Cochrane Database Syst Rev. 2011 Mar 16;(3):CD007871
- Bolliger D, Seeberger MD, Tanaka KA. Principles and practice of thromboelastography in clinical coagulation management and transfusion practice. Transfus Med Rev. 2012 Jan;26(1):1-13
- da Luz LT, Nascimento B, Rizoli S. Thrombelastography (TEG(R)): practical considerations on its clinical use in trauma resuscitation. Scand J Trauma Resusc Emerg Med. 2013 Apr 16;21(1):29.
- Ganter MT, Hofer CK. Coagulation monitoring: current techniques and clinical use of viscoelastic point-of-care coagulation devices. Anesth Analg. 2008 May;106(5):1366-75
- Hunt H, Stanworth S, Curry N, Woolley T, Cooper C, Ukoumunne O, Zhelev Z, Hyde C. TEG and ROTEM for diagnosing trauma‑induced coagulopathy (disorder of the clotting system) in adult trauma patients with bleeding. Cochcane Review. 2015
- Tapia NM et al. TEG-guided resuscitation is superior to standardized MTP resuscitation in massively transfused penetrating trauma patients. J Trauma Acute Care Surg. 2013;74:378-386.
- Thakur M, Ahmed AB. A review of thromboelastography. Int J Periop Ultrasound Appl Technol 2012;1(1):25-29.
- Whiting D, DiNardo JA. TEG and ROTEM: technology and clinical applications. Am J Hematol. 2014 Feb;89(2):228-32. doi: 10.1002/ajh.23599. PMID: 24123050. [article]
FOAM and web resources
- ICN — SMACC: Hurn on TEG/ROTEM in the Real World (2013)
- Joe Elbeery on Youtube — TEG basics video (2013)
- Maryland CCP — The Use of TEG & Goal Directed Blood Component Therapy by John Walsh (2013)
- Practical-Hemostasis.com — TEG and ROTEM
- The websites for the ROTEM and TEG provide a comprehensive explanation of the waveforms generated in various disorders.

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

Brilliant article
Explaining this complex topic so simply
I loved it.
Thank you
Are there any additional / newer technology(ies) available today?
[…] Life in the Fast Lane on POC coagulation testing […]