Paediatric ECG: Stepwise approach
- Normal paediatric ECG
- Paediatric ECG lead placement
- Stepwise assessment of the paediatric ECG
- Common paediatric arrhythmias
Stepwise assessment of the paediatric ECG
2.1 Rhythm
Sinus: Atrial depolarisation starts from the sinoatrial node. This requires:
- P wave preceding each QRS complex, with a constant PR interval
- Normal P wave axis (zero to +90 degrees), i.e. P wave is upright in leads I and aVF
Non-sinus: Some atrial rhythms may have P waves in front of every QRS but with an abnormal P axis (inverted in lead II).
Note prominent sinus arrhythmia is commonly seen in children.
2.2. Rate
As per rate interpretation for adults.
Heart rates are highest in neonates and infants and decrease with age. The younger the child, the higher the metabolic rate and lower vagal tone:
- Newborn: 110 – 150 bpm
- 2 years: 85 – 125 bpm
- 4 years: 75 – 115 bpm
- > 6 years: 60 – 100 bpm
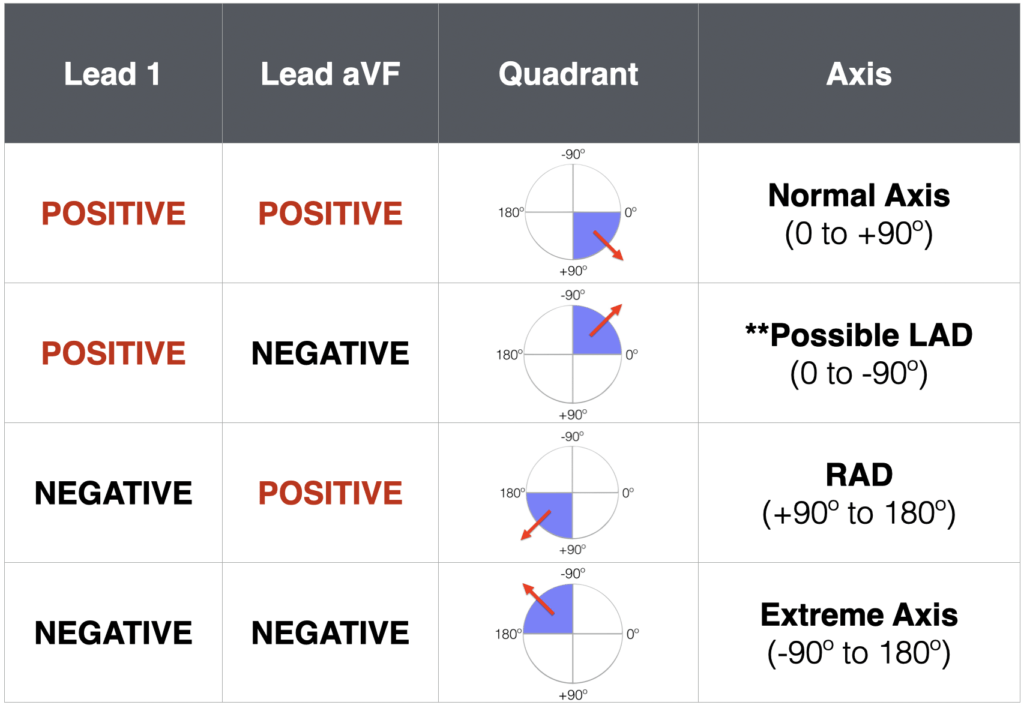
2.3 QRS axis
As per adult interpretation, calculated using the hexaxial reference system that shows the frontal view of the electrical activity of the heart via the six limb leads.
Normal QRS axis varies with age:
- 1 week – 1 month: + 110° (range +30° to +180°)
- 1 month – 3 months: + 70° (range +10° to +125°)
- 3 months – 3 years: + 60° (range +10° to +110°)
- Over 3 years: + 60° (range +20° to +120°)
- Adult: + 50° (range -30° to 105°)
Initial right ventricular (RV) dominance
In utero, blood is shunted away from the pulmonary vasculature leading to higher pulmonary pressures and a relatively larger and thicker right ventricle. Right axis deviation is thus a normal finding at birth, and usually resolves by 6 months of age.
A north-west axis (-90 to -180 degrees) is seen at birth with AV canal or ostium primum atrial septal defects
2.4 ECG intervals
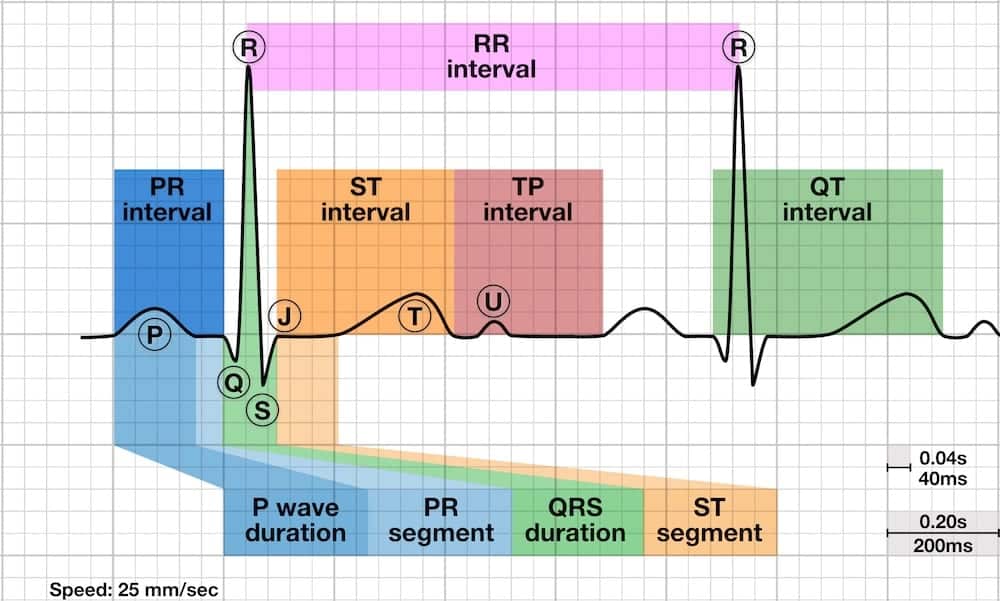
- PR interval and QRS duration are shorter at birth due to smaller cardiac size
- Normal QT interval is slightly prolonged at birth
PR Interval
The normal PR interval varies with age and heart rate:

Prolonged PR interval (first degree heart block) may be normal or be seen in:
- Viral or rheumatic myocarditis and other myocardial dysfunctions
- Certain congenital heart disease (Ebsteins, ECD, ASD)
- Digitalis toxicity
- Hyperkalaemia
Short PR interval occurs in:
- Pre-excitation (eg Wolff-Parkinson-White)
- Glycogen storage disease
Variable PR interval occurs in:
- Wandering atrial pacemaker
- Wenckebach (Mobitz type 1) second degree heart block
QRS Duration
QRS duration varies with age:
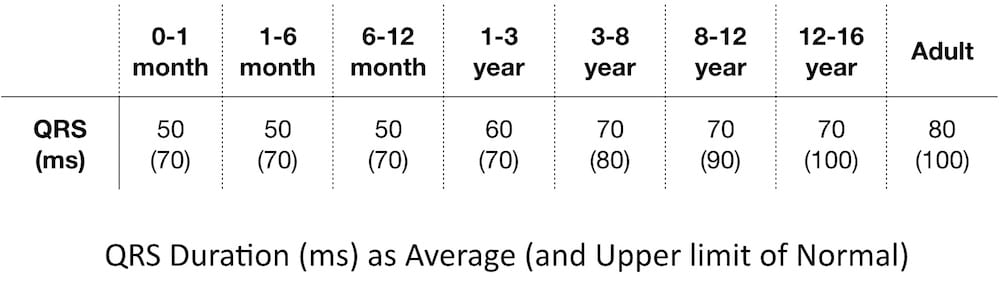
Prolonged QRS is characteristic of ventricular conduction disturbances:
- Bundle branch blocks
- Pre-excitation conditions (eg WPW)
- Intraventricular block
- Ventricular arrhythmias
QT Interval
QT interval varies with heart rate:
Bazett formula is used to correct the QT for HR:
- QTc = QT measured / (√R–R interval)
Normal QTc
- Infants less than 6 months = < 490 ms
- Older than 6 months = < 440 ms
QTc is prolonged in:
- Hypocalcaemia
- Myocarditis
- Long QT syndromes such as Romano-Ward
- Head injury
- Drugs
QTc is short in:
- Hypercalcaemia
- Digitalis effect
- Congenital short QT syndrome
2.5 P wave amplitude and duration
- Normal P-wave amplitude is < 3 mm (tall P waves = right atrial enlargement)
- Normal P wave duration is < 0.09 seconds in children and < 0.07 seconds in infants (wide P waves = left atrial enlargement)
- A combination of tall and wide P waves occurs in combined atrial hypertophy
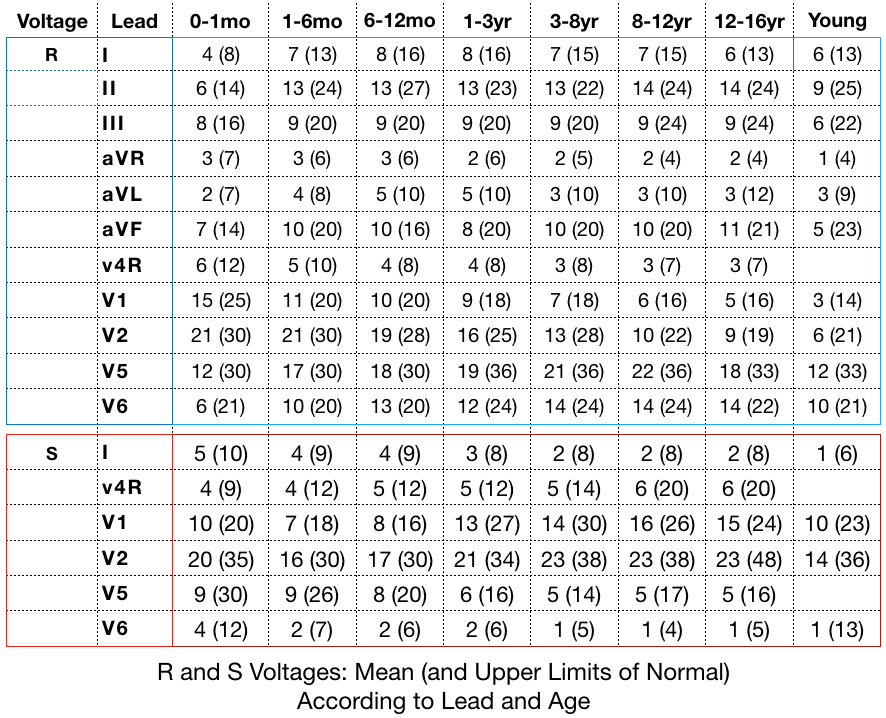
2.6 QRS amplitude (voltages)
High QRS amplitudes are found in:
- Ventricular hypertrophy
- Ventricular conduction disturbances eg BBB’s, WPW
Low QRS amplitudes are seen in:
- Pericarditis
- Myocarditis
- Hypothyroidism
- Normal newborns
Ventricular hypertrophy
Ventricular hypertrophy produces changes in one or more of the following areas: the QRS axis, the QRS voltages, the R/S ratio and/or the T axis.
The presence of ECG features of left ventricular hypertrophy in a paediatric patient should prompt the clinician to look for other ECG and clinical features of hypertrophic cardiomyopathy and investigate as appropriate.
Right ventricular hypertrophy
Axis: RAD for the patients age
Voltages:
- Tall R waves (greater than limits for patient’s age) in right-sided leads V4R and V1
- Deep S waves (greater than limits for patient’s age) in left-sided leads V5 and V6
R/S ratio: Abnormal R/S ratio in favour of RVH.
- Increased R/S ratio (greater than upper limits for child’s age) in V1-2
- R/S ratio < 1 in V6 (after one month of age)
Abnormal T waves: Upright T waves in V1 and V4R in children 3 days to 6 years (provided that T waves are normal elsewhere, i.e. upright in V6). This is evidence alone of significant RVH.
Abnormal Q waves: qR pattern in V1 (small Q wave, tall R wave) = highly specific for RVH.
Left ventricular hypertrophy
Axis: LAD for the patients age (marked LAD is rare with LVH).
Voltages:
- Tall R waves in the left-sided leads V5 and V6 (greater than limits for patient’s age)
- Deep S waves in the right-sided leads V4R and V1 (greater than limits for patient’s age)
R/S ratio:
- Abnormal R/S ratio in favour of LV
- Decreased R/S ratio in V1-2 (less than upper limits for child’s age)
Abnormal Q waves in V5 and V6
Inverted T waves in I and aVL (LV strain pattern)
Biventricular hypertrophy
- Positive voltage criteria for RVH and LVH (with normal QRS duration)
- Positive voltage criteria for RVH or LVH and relatively large voltages for other ventricle
- Large equiphasic QRS complexes in two or more limb leads and in mid-precordial leads (V2-5)
Evans Rules
Small chest walls exaggerate precordial voltages. Evans et al proposed a practical approach to evaluation:
Abnormal Left Ventricular Large Voltage (“LVH”)
Use only V6 (the left most precordial lead)
- If R wave of V6 intersects with baseline of V5, this is ABNORMAL
Abnormal Right Ventricular Large Voltage (“RVH”)
Use only V1 (the right most precordial lead)
- Upright T wave in V1: In first week of life is NORMAL. Between week 1 and adolescence this is ABNORMAL
- RSR’ in V1: If R’ is taller than R – this is ABNORMAL
- Pure R wave in V1: If child > 6 months old – this is ABNORMAL
2.7 Q waves
Normal Q waves:
- Narrow (average 0.02 seconds and less than 0.03 seconds)
- Usually less than 5mm deep in left precordial leads and aVF
- May be as deep as 8mm in lead III in children younger than 3 years
Q waves are abnormal if they are:
- Present in the right precordial leads ie V1 (eg severe RVH)
- Absent in the left precordial leads (e.g. LBBB)
- Abnormally deep (ventricular hypertrophy) – look for “dagger” Q waves in leads I, aVL and V5-6, often seen in hypertrophic cardiomyopathy
- Abnormally deep and wide (myocardial infarction or fibrosis)
2.8 ST segment
Interpretation is as per adults – the normal ST segment is isoelectric. Elevation or depression is judged in relation to the TP segment.
Some ST changes may be normal:
- J-point depression: the J point (junction between the QRS and ST segment) is depressed without sustained ST depression, i.e. upsloping ST depression.
- Benign early repolarisation is a common finding in adolescents: the ST segment is elevated and concave in leads with an upright T wave

Others are pathological:
- Coved or saddle-back ST elevation in V1-3 should raise concern for Brugada syndrome
- A sustained horizontal ST segment depression 0.08 sec or longer is abnormal
Pathological ST segment changes are commonly associated with T wave changes and occur in:
- Pericarditis
- Myocardial ischaemia or infarction
- Severe ventricular hypertrophy (ventricular strain pattern)
- Digitalis effect
2.9 T Waves
The precordial T-wave configuration changes over time:
- For the first week of life, T waves are upright throughout the precordial leads
- After the first week, the T waves become inverted in V1-3 (= the “juvenile T-wave pattern”)
- This T-wave inversion usually remains until ~ age 8; thereafter the T waves become upright
- However, the juvenile T-wave pattern can persist into adolescence and early adulthood (= “persistent juvenile T waves”)
Tall, peaked T waves are seen in:
Flat T waves are seen in:
- Normal newborns
- Hypothyroidism
- Hypokalaemia
- Digitalis
- Pericarditis
- Myocarditis
- Myocardial ischaemia
Large, deeply inverted T waves are seen with:
- Raised intracranial pressure (e.g. intracranial haemorrhage, traumatic brain injury)
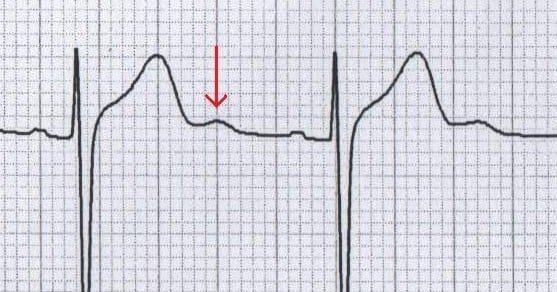
2.10 U waves
U Waves are the extra positive deflection at the end of a T wave. Most common causes:
- Hypokalaemia
- Normal finding at slower heart rates (e.g. sinus bradycardia)
Related topics
- Paediatric ECG Basics
- Normal paediatric ECG
- Paediatric lead placement
- Common paediatric arrhythmias
- ECG approach in syncope
References
- Paediatric Electrocardiography by Steve Goodacre and Karen McLeod, from the BMJ’s “ABC of Clinical Electrocardiography” series (2002)
- O’Connor M, McDaniel N, Brady WJ. The pediatric electrocardiogram. Part I: Age-related interpretation. Am J Emerg Med. 2008 Feb;26(2):221-8
- Evans WN1, Acherman RJ, Mayman GA, Rollins RC, Kip KT. Simplified pediatric electrocardiogram interpretation. Clin Pediatr (Phila). 2010 Apr;49(4):363-72.
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner